Three challenges to mobilising One Health collaborations
Published on 22/11/2021

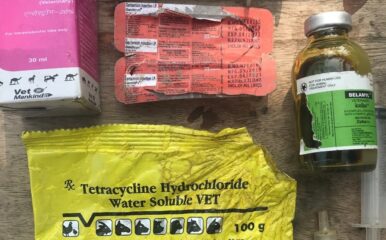
PxHere
View this page in:
VietnameseWhile many articles explain what is One Health, and its importance for addressing antimicrobial resistance (AMR), what is often missing from discussion is why One Health (and similar) multisector partnerships are hard to devise and implement. This, despite repeated calls for such One Health partnerships.
On the occasion of this World Antimicrobial Awareness Week, I would like to draw your attention to what I feel is the single-most important foundational weakness in global AMR control efforts – which is the difficulty in mobilising multisector One Health collaborations. I draw upon a recently published paper examining the literature around multisectoral partnerships.
AMR is a complex problem which is driven by activities from a wide range of actors and it impacts them unequally. Indeed, for some stakeholders, AMR might not even be seen as a problem, when they are motivated by more immediate and pressing concerns, such as maintaining their competitiveness in a crowded low-margin market – be it the case of informal health practitioners in India, poultry producers in Vietnam or shrimp farmers in Bangladesh.
In such a situation, getting sectors to work together around narrowly defined AMR outcomes remains a challenge.
The WHO Global Action Plan and LSHTM Roadmap for AMR surveillance both accord importance to One Health collaborations. They have inspired the development of National Action Plans that propose an institutional framework to encourage data analysis and decision making around AMR to cut across the animal, human and environment sectors.
However, the reality for most countries is that getting sectors to actually work together (to develop common databases, share information, undertake joint planning and coordinated response, and more) remains a challenge – as evidenced by the countries themselves in the Tripartite Antimicrobial Resistance (AMR) Country Self-assessment Survey (TrACSS).
I believe a reason why One Health remains difficult to operationalise is our inability to recognise the political dynamics underpinning multisector partnerships. One Health is too often presented as a technocratic fix for a policy goal that does not take into account the social, institutional and individual dynamics that influence partnerships.
On the other hand, while it is all very good to say that we should recognise the politics of One Health, how can this translate into practice? I would like to think that this paper offers some answers. Drawing upon our recently published review of collaboration literature, I demonstrate key myths of multisector partnerships and how can they be addressed. These are as follows:
International guidelines, including those from the Food and Agricultural Organization (FAO), the World Organisation for Animal Health (OIE) and World Health Organization (WHO) tripartite and from the World Bank, emphasise the need to adapt One Health to local context. However, in the absence of a lexicon/typology, they fail to specify how country managers can do so.
In our paper, my co-authors and I propose several different ways in which multisector partnerships might be categorised. We propose, for instance, that multisector partnerships be categorised on the basis of scale, scope, formality and strength.
Only once we start describing One Health partnerships on the basis of their characteristics, can we then have a more nuanced discussion on the type of One Health that best suits a given context. Such a typology can then be used to offer a menu of options to countries and allow them to choose the type of One Health that suits their needs best.
Different partners have different mandates, incentives, interests and agency. AMR regulation in human health might involve surveillance and regulation of antimicrobial use. However, farmers in highly competitive poultry or aquaculture sectors might have a different understanding of the use of antimicrobials and their nodal ministries might have limited capacities for generating data or influencing practice in the absence of major market interventions.
Instead of pushing for human health outcomes as a ‘shared goal’ of One Health collaboration, it might be useful to ask about the expectations of other sectors from a shared enterprise such as One Health.
Continuing from the last point, there needs to be some room for the One Health partnerships to manoeuvre and adapt their goals to respond to partner needs or to changing external circumstances. Rigid ringfencing of objectives for One Health collaborations, such as AMR committees, might end up limiting the effectiveness of One Health collaborations. Some flexibility to collaborations will likely lead to their increased resilience to sustain over a period of time.
The underlying logic of much of One Health discourse appears to be, “if we can just bring people together in a room regularly, productive partnerships and collaborations will automatically flow”. As anyone who has been stuck in long meetings will attest, that is not always a given!
However, as our analysis points out, the solution might ultimately be similar to the techniques we use to develop collaborative discussions at an individual level; viz. recognising that people have different points of view, empathising with their concerns and having the flexibility to adapt to partner needs.